Utilizing Nurse Case Managers for Workers Compensation Claims
One of the biggest challenges that the workers’ compensation industry faces today is the continuous rise in medical costs. As a result, the industry fights for improved efficiencies and cost containment, and injured workers can often get lost in the shuffle. Until now, most employers have focused on containing costs and reducing days lost, representing a more transaction-centric approach. However, experts now say that changing the primary focus to supporting the injured worker can improve outcomes for all parties involved in a claim.1
Utilizing a nurse case manager in the right instances can avert delays in a timely return to work.
By focusing on the injured worker and the improvement of their health and wellness, employers can shift their focus back to their most important goal: making people healthy again. Behind every claim is an injured worker seeking to get better. If a nurse case manager is engaged in a workers’ compensation claim, they have the opportunity to deliver multiple benefits and build trust with the injured worker to ultimately support a timely recovery. In order to be an advocate in an injured worker’s journey to recovery, a nurse case manager will facilitate their medical needs and ensure a continuous flow of communication between them, the injured worker, the provider, claim adjuster and the employer. Serving as an injured worker’s advocate by placing the injured worker first not only empowers the worker throughout the claims process, but it also reinforces the “people first” philosophy manifested in the “advocacy-based” claims model—a catch-phrase that is growing in popularity within the industry.  In short, as an industry, we need to realign ourselves with the principle that healthcare was founded upon: protecting the patient's interests, prioritizing them first. The primary purpose of workers’ compensation is to get injured workers back to work as quickly as possible and ensure appropriate care is rendered at the appropriate time. When that fundamental principle is the focus, reduced costs generally follow.
In short, as an industry, we need to realign ourselves with the principle that healthcare was founded upon: protecting the patient's interests, prioritizing them first. The primary purpose of workers’ compensation is to get injured workers back to work as quickly as possible and ensure appropriate care is rendered at the appropriate time. When that fundamental principle is the focus, reduced costs generally follow.
Moving Toward Better Timing to Address the Challenge Sooner
In 2015, the U.S. Bureau of Labor Statistics reported 2.9 million nonfatal workplace injuries occurred that year. Of this, over 50 percent of the injured workers experienced time lost from work.2 Consequently, when expert analysis is done, the findings approximate that 75 percent of employees return to work after 12 weeks of lost work time, but only 20 percent return after a year. Based off these numbers, the observation turns out to be: the longer an injured worker is out of commission, the more likely it is that they don’t return to work at all. As a result, there is an imperative to helping injured workers avoid long delays in returning to work. According to industry statistics, only about 10 percent of U.S. workers’ compensation claims are utilizing nurse case managers.3 Although case management may not be necessary for all workers’ compensation claims, utilizing a nurse case manager in the right instances can avert delays in a timely return to work. 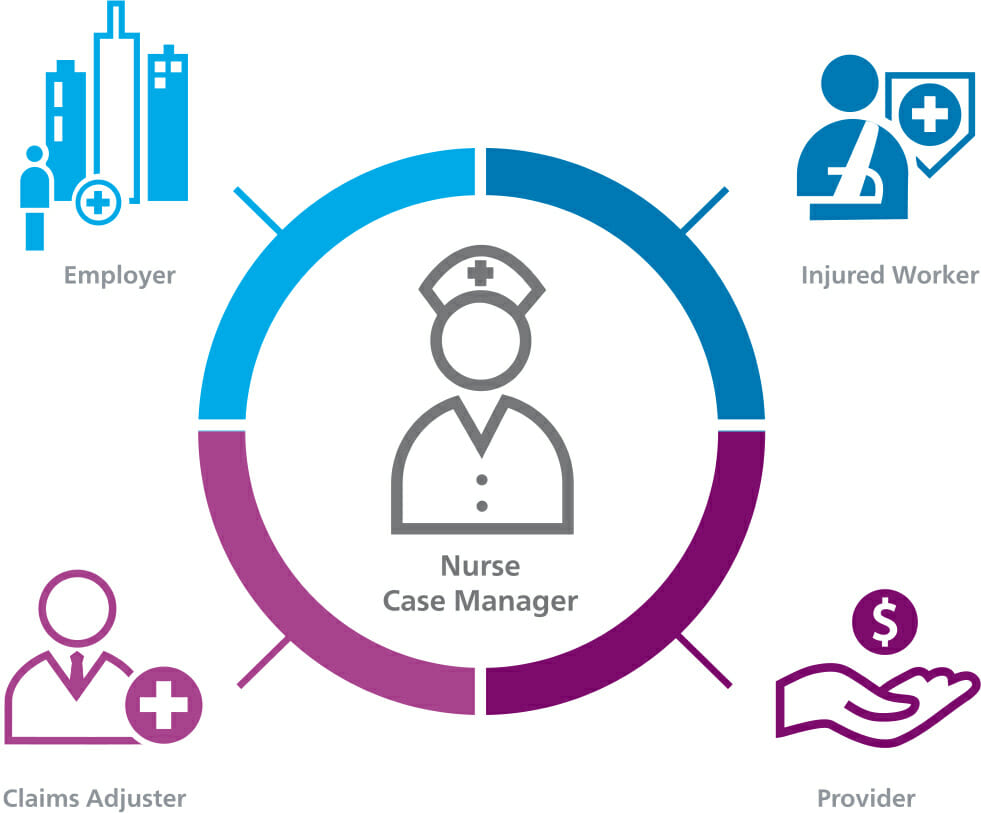 The most critical point in time to effect the outcomes in medical care, claim costs and return to optimum function and work is immediately after injury. Proactively assigning a nurse case manager to help guide the injured worker early in the claims process can empower and accelerate a return-to-work plan to avoid delays in progress.
The most critical point in time to effect the outcomes in medical care, claim costs and return to optimum function and work is immediately after injury. Proactively assigning a nurse case manager to help guide the injured worker early in the claims process can empower and accelerate a return-to-work plan to avoid delays in progress.
Engaging a nurse case manager on a claim can save an average of $6,100 in medical and indemnity costs, resulting in an 8:1 ROI.
In addition, there is the potential opportunity to realize cost efficiencies on medical spend should a case be referred to case management in a timely manner. Engaging a nurse case manager on a claim can save an average of $6,100 in medical and indemnity costs, resulting in an 8:1 ROI.4 Time delays in referring a claim to case management have been found to increase claim costs 18 percent on cases reported at two weeks, as opposed to those reported at one week.5
Combating Costs
In an ideal world, First Reports of Injury (FROI) or the first notice of treatment of an injured worker should be forwarded to the medical management organization for case management triage. Realizing that not every case warrants a nurse at the beginning, employers and carriers benefit from having a “trigger” list of injuries on which it would be advantageous to enlist early case management. The key to cost containment is not to prohibit workers from care or provide less desirable care, but rather to ensure the right care is provided at the right time. Early case management facilitates treatment:
- Provided within networks, if applicable
- Provided within evidenced-based guidelines
- Education to the worker informing them of successful outcome expectations, including return to work (RTW) time points
Employees who are injured on the job tend to withdraw from their co-workers and supervisors when they are off work. Whether it be television advertisements about attorneys or the worker speaking to a neighbor, many injured workers seek legal advice and representation during the course of their rehabilitation, potentially adding significant costs and delays to the case. Early case management intervention promotes healthier relationships between all parties because the worker feels that they have someone to advocate for them. The nurse can explain the treatment in layman’s terms, facilitate earlier appointments, and collaborate with the physician resulting in more timely treatment, which typically results in a shorten time for which a claim is open.
Early case management intervention promotes healthier relationships between all parties.
Many times case management is compared to a train. If the nurse gets on at the beginning of the trip the case is far less likely to derail. If a nurse is assigned to a case months or years after the injury there is often little to do but pick up the pieces and attempt to move to resolution. Cost containment should commence at the beginning of the trip to help maximize the realization of positive outcomes. Collaboration with other units within the organization such as utilization review and bill review, as well as access to external claims systems are important components of this trip. Nurse case managers depend on documentation from these units to aid them in compiling a complete picture of the case.
Smarter Data Integration Offers Fuller Visibility into the Claim
Integration between bill review and managed care is an important component of effective case management. Not all claims will warrant a nurse case manager, but among those that do, advanced workers' comp claims software technology solutions can help provide visibility into scenarios where a workers’ compensation claim may benefit from medical professional guidance. Claims should be evaluated for case management intervention using multiple triggers. Collaborations between bill review and managed care, two typically “siloed” work streams, can provide insights into an “at-risk” claim. If an insurer has access to a staff of nurses with years of certified medical experience, not only can they identify and address clinical issues an injured worker may be facing, but they can also successfully intervene with case management services to make sure the injured worker reaches optimal medical improvement. These critical synergies support employers and payors to proactively monitor and identify suboptimal pathways throughout the claims journey. As a result, cost and process efficiencies are shown to improve for all stakeholders involved. While the constantly changing nature of healthcare continues to evolve to drive new solutions to address the many challenges within the workers’ compensation industry, the goals remain the same for nurse case managers – to provide high quality care and cost-effective solutions to injured workers. By achieving these goals, nurse case managers can empower them to see improved value in their life at work and at home. When workers’ compensation carriers begin to programmatically utilize nurse case managers, it can start an integrated system of delivering high quality patient care along with cost-containing claims efficiencies, allowing them to provide more trusting services and drive better outcomes. 

