2019 CMS Medicare Payments: Proposed Changes and What They Mean for P&C Insurers
Several states in auto and workers’ compensation claims administration have adopted the Centers of Medicare and Medicaid Services’ (CMS) fee schedules and/or rules for payment of claims. The methodologies employed by CMS in provider billing and payment are typically either mandated by statute or become standards for appropriate billing and payment of claims. When Medicare adds new codes or proposes changes to fee schedules, Mitchell prepares for these changes by reviewing the proposed changes and how they could affect the Property and Casualty industry (P&C). Changes that occur with CMS rules could have a significant impact in those states for auto and workers’ compensation that have adopted the Medicare fee schedules. The allowable commentary from Mitchell to CMS during the public comment periods is an optimal way to be heard by this administration. In July 2018, CMS made proposals for changes to the 2019 Medicare Physician Fee Schedule (MPFS) and Quality Payment Program with the public comment period ending September 10, 2018. Under the proposed 2019 MPFS, CMS will be making changes to:
- Remote Patient Monitoring
- Evaluation and Management coding and document requirements
What is Remote Patient Monitoring?
Often abbreviated as RPM, remote patient monitoring is exactly what it sounds like: the ability to monitor a patient from a remote location. In today’s age of advanced technologies, healthcare professionals can now use the latest advances in information technology to collect data from a patient, remotely deliver them a method of healthcare, and monitor patient behavior from a distance.
Remote patient monitoring is exactly what it sounds like: the ability to monitor a patient from a remote location.
Does RPM give additional information to the treating provider that they would otherwise not have? Will having this additional information and ability assist with patient care, specifically in the P&C industry? These and other questions will be answered if the new rules are approved after evaluation by CMS, and the patterns of billing are observed over time.
What is Telehealth? How is RPM Different?
RPM often gets confused with telehealth, and so we need to eliminate some confusion between the two terms. Simply put, telehealth is where the provider can actually treat a patient remotely and is typically used as a broader term that refers to the entire industry, methodology and technologies that enable a specific type of healthcare. RPM, on the other hand, is monitoring a patient by collecting a wide range of health data. In the workers’ compensation industry, RPM can provide benefits such as recording an injured worker’s actual activity level—including diet, exercise and potential health and life-threatening situations. This type of data can be valuable to health professionals, since they can modify and update a patient’s treatment plan based on the information they receive. Providers with access to RPM can have actual data versus information that is self-reported from the patient; but which one is telling the truth? In today’s world where medication monitoring—especially adherence—is dependent upon the patients’ information, RPM can assist with the monitoring. It can also assist the patient by providing “reminders” to be vigilant in following provider instructions.
CMS’s Proposal
As a start to the expansion of RPM coding, CMS unbundled the CPT code 99091, effective January 2018. This change meant that eligible providers can bill to receive separate reimbursement “for the time spent on collection and interpretation of health data that is generated by a patient remotely, digitally stored and transmitted to the provider at a minimum of 30 minutes of time.” This was a big change—in prior CMS rules, remote tasks could not be billed for many situations. As a result of the January 2018 change, services that fall under the new CPT code 99091 can now be billed once per patient during the same 30-day service period. The new proposal for 2019 is part of the Advancing Virtual Care program proposed by CMS. According to CMS, the goal of the program is to support access to care using communication technology. CMS is proposing to (CMS, 2019):
- Pay clinicians for virtual check-ins—brief, non-face-to-face assessments via communication technology;
- Pay Rural Health Clinics (RHCs) and Federally Qualitied Health Centers (FQHCs) for communication technology-based services and remote evaluation services that are furnished by a RHC or GQHC practitioner when there is no associated billable visit;
- Pay clinicians for remote evaluation of patient-submitted photos or recorded video; and
- Expand Medicare telehealth services to include prolonged preventive services.
RPM Billing
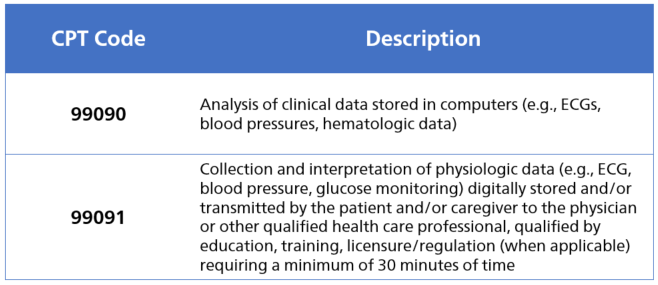
Current codes used for billing RPM services are:
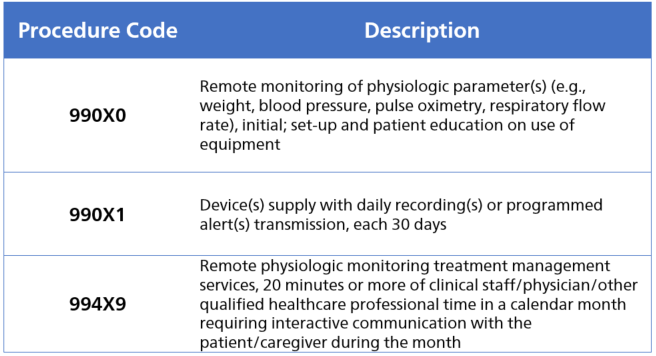
CMS’s proposal for new codes in 2019 are (X is a placeholder):
These new codes focus on the collection of patient-generated health data remotely, through devices and mobile health platforms that connect to the primary care provider or care team. This data can either be collected and sent by the patient or gathered by connected devices and automatically sent to the provider without the patient’s participation.
Mitchell Perspective
As with any new CMS rules, Mitchell reviews the changes to determine how they might affect the billing and payment of claims within the P&C industry. Patients in P&C frequently receive hands-on treatments as a part of their care. New codes and rules are often confusing to the provider’s office staff, and that confusion can translate into improper coding and billing to the insurance carrier. Insurance carriers will likely also have questions about the new codes, especially during the initial period of transition. After reviewing the proposed changes around RPM, we posted a few questions to CMS during the allowable comment period. Here are the questions Mitchell asked:
- How should bill review companies handle RPM codes billed by chiropractors, physical therapists, occupational therapists or other hands-on providers? Our concern is that the new codes will become “add-on” fees and new costs that were normally considered as part of the Evaluation and Management codes, or included in other visit codes as part of questioning the patient.
- What will the standards of monitoring include and what type of communication is acceptable? We know from previous rules that if CMS is not specific we may see a wide range of communications submitted. We are unsure if data from a Fitbit activity tracker or other personal wearables will be part of this communication.
- What limitations will be placed on the reporting? We need to understand if the reporting is specific to the code description only.
Summary of RPM
What we’ve heard is that many practitioners have trepidation around the use of communication devices, since most of the technology involved in RMP has not been proven reliable. Practitioners are not ready to trust the data from these devices and technologies as accurate enough to diagnose or treat. In addition, many of these devices collect enormous amounts of data and it is questionable whether the provider will have enough time to review the amount of data sent for every patient. On the other hand, providers have been in need of more data to monitor patients with chronic conditions.
For the injured worker, instead of self-reporting that they are adhering to the rehab plan, RPM tracking will, in theory, be able to monitor and track this automatically.
One positive associated with the increased use of RPM is that having the data available for medication and lifestyle changes could potentially lead to huge benefits for patients. For the injured worker, instead of self-reporting that they are adhering to the rehab plan, RPM tracking will, in theory, be able to monitor and track this automatically. This kind of automation helps expedite communications and data to “potentially lead to more adherence to treatment plans and faster return to work.”4
Evaluation and Management Services
CMS is also proposing major changes to the Medicare Fee Schedule Evaluation and Management (E/M) reimbursement model for office and outpatient services. The proposal would create a new single blended payment regardless of what E/M level was performed. Additionally, CMS is relaxing the E/M code documentation requirements. The proposed CMS Physician Fee Schedule would pay a flat fee for levels 2 through 5. The suggested payment model will treat complex patient’s reimbursement at a “level 5” which would pay the same as for a patient receiving a “level 2” visit. The overhaul of the E/M services was in response to the “Patients over Paperwork” initiative. The E/M services are considered to be one of the areas consuming too much practitioner time in creating and updating documentation considered to be excessive and unnecessarily burdensome.
CMS is also proposing major changes to the Medicare Fee Schedule Evaluation and Management (E/M) reimbursement model for office and outpatient services. The proposal would create a new single blended payment regardless of what E/M level was performed.
It is important to note that the new rules are specific to CMS payments at this time and not part of the American Medical Association (AMA) guidelines for billing E/M Services. This may have some confusing aspects, especially in states that have adopted the Medicare Physician Fee Schedule in P&C. A great example is Pennsylvania, a no-fault state which utilizes Medicare rules in the application of the MPFS. In Florida’s PIP coverage, many of the CMS rules are not followed but the Medicare Physician Fee Schedule is utilized as a standalone.
Billing of Evaluation and Management
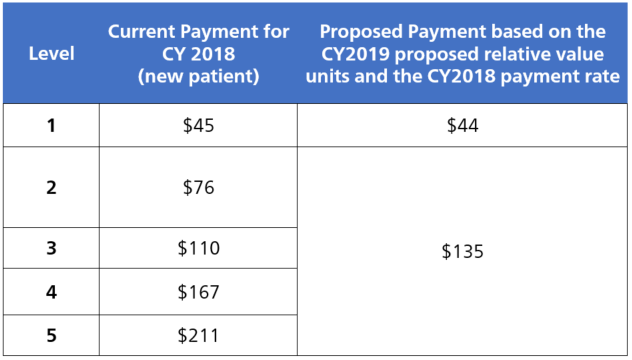
CMS is proposing the following schedule for 2019 for “new” patient visits:
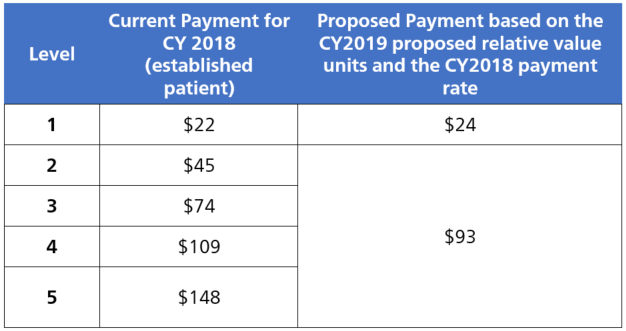
The following is the proposed fee schedule for established E/M services:
The appropriate payments will be based upon the above rates, plus add-on codes (G Codes yet to be determined) that will enhance the payment for the E/M Services. For Medicare billing the documentation for the E/M service will only need to be at the Level 2 service for History, Exam and Medical Decision Making to be paid for any level of service. As a result, “time” will become one of the governing measurements of the appropriate level of service due to the add-on code enhancements. CMS is proposing to create a Healthcare Common Procedure Coding System (HCPCS) G-code for primary care services and add-on codes that should be listed separately in addition to an established patient evaluation and management visit. Additional payment codes include:
- Proposing ~$5 add-on payment to recognize additional resources to address inherent complexity in E/M visits associated with primary care services.
- Proposing ~$14 add-on payment to recognize additional resources to address inherent visit complexity in E/M visits associated with certain non-procedural based care.
- Proposing a multiple procedure payment adjustment that would reduce the payment when an E/M visit is furnished in combination with a procedure on the same day.
- Proposing a ~$67 add-on payment for a 30 minute prolonged E/M visit.
Mitchell Perspective
In the P&C industry, E/M services control the top 15 procedure codes utilized, and could have a greater impact on providers in casualty from a payment perspective. We are currently assessing the impact based upon past data performance (not predicting provider behavior changes). Provider groups, such as the AMA, are concerned that payments to specialists who were billing at a higher level will be combined into this new methodology (American Medical Association, 2018). In addition, CMS is proposing add-on codes which can be an area of concern due to the lack of documentation required for reporting the E/M services. There is no clear definition of when it is appropriate to use the add-on codes for additional reimbursement yet, which opens diverse billing practices from providers. These new proposals are CMS rules and payment guidelines used by providers to bill CMS, however, these new HCPCS codes will be available to all providers to use outside of the CMS system in addition to the fee schedule states. Florida PIP is of specific concern due to the language in the statute that directs payment of services to be no less than the 2007 CMS MPFS. While it is a clear comparison, code to code – the add-on codes cause complications in the comparison due to the variability in the usage. Although payments for procedure codes individually have not been different for specialties, the E/M services were utilized at higher levels for treating conditions requiring more services. Due to the blending of levels 2–5, it may cause specialty practices added concern for payments. As referenced by the AMA, the more complex provider visit (i.e., Neurosurgeon) who normally bill higher-level E/M service codes will no longer be paid a different rate than a level 2. A question to CMS from Mitchell during the comment period in relation to the usage of the add-on codes was: Will there be a specific specialty rule?
Summary of Evaluation and Management Services
From the documentation guidelines, it is clear that E/M services cause provider offices to perform a great deal of administrative work today. It is also clear that it requires insurers like CMS to spend additional resources to review the documentation provided by the practitioners. Creating an environment of billing where time is the determining factor regardless of the severity of the illness can cause the prices for total office visit, (E/M plus add-on code usage) to rise. Contrary to previous documentation guidelines, these proposed changes provide that the value of healthcare is based on time rather than the quality of services rendered that were previously documented in the E/M guidelines. In P&C claim adjudication, most states require the AMA guidelines are followed for the use of CPT codes billed. The proposed CMS changes do not support the AMA guidelines for using appropriate CPT codes as they only apply to CMS payments in the proposal. Many states in P&C have adopted the CMS MPFS for payment of claims but not the rules which can add to confusion for providers billing and what they anticipate being paid. After all comments have been evaluated, CMS will publish the approved rules November 2018 for all proposed changes to the MPFS.