Are You Paying for Mistakes? The Impact of Errors in Workers' Comp Medical Billing
Workers' Compensation Medical Billing Errors Could be Costing Payors Thousands of Dollars.
This article is the first in a three part series about auditing workers’ compensation medical bills for errors and abuses
There is one question insurers and other payors should be asking themselves: Am I paying for billing mistakes? Incorrect billing costs payors millions of dollars across the industry because many of those payors are paying bills with errors in full. A recent article from HuffPost references a University of Minnesota professor’s research that projects 30-40 percent of medical bills contain errors. A report from the Medical Billing Advocates of America estimates that as many as 80 percent of all medical bills include incorrect information. Another study from NerdWallet found that about 50 percent of the Medicare claims they examined involved some type of inaccuracy. Though the precise rate of billing errors is unknown, one thing is certain—most payors are paying for mistakes and many don’t even know it.
A Market-Wide Problem
This problem is not limited to group health or Medicare. Mitchell studies confirm that billing errors on workers’ compensation claims are also prevalent. For example, one of our analyses found equally concerning results—35 percent of the hundreds of thousands of workers’ compensation bills that we audited contained some type of billing error. Our analysis shows the most common types of issues on the set of bills we analyzed were:
- Edits
- CCI issues (inappropriate coding)
- Unbundling (billing for multiple procedures covered by one comprehensive code)
- MUE errors (medically unlikely edits)
- Other
Error Types
The chart below provides an overview of how frequently each of these types of errors occurred in our analysis. 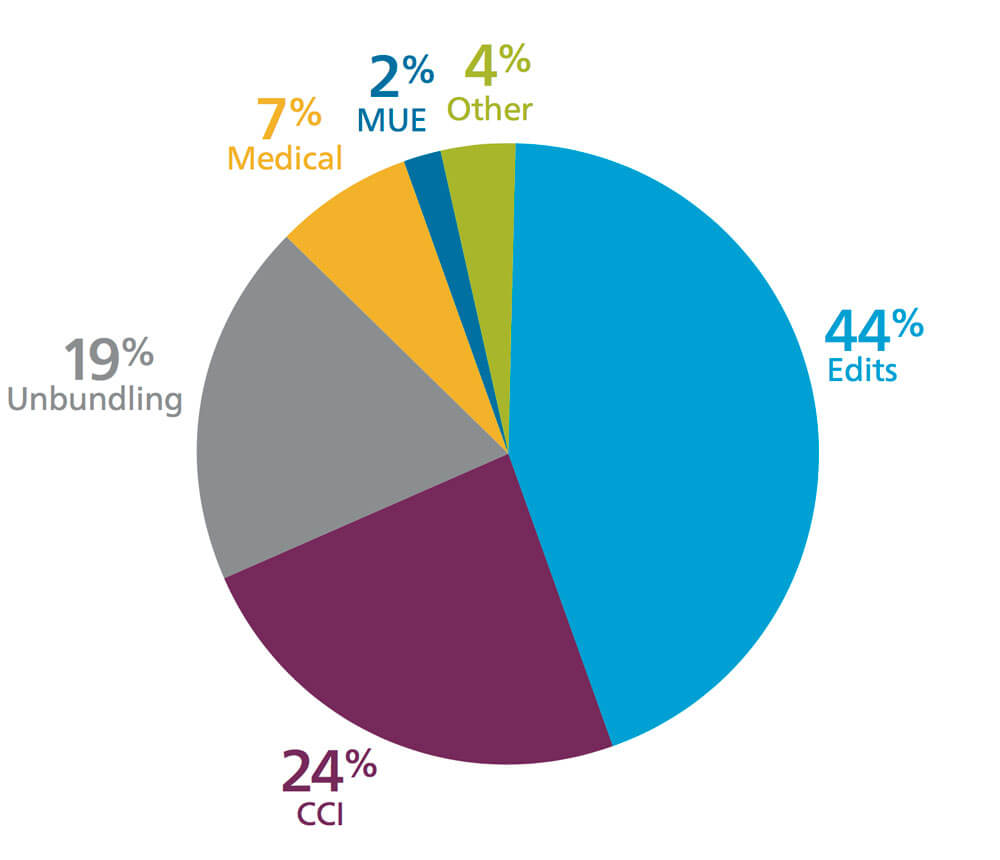

How Do These Errors Happen?
Processing a bill requires many different people and the potential for errors increases every time a new person or organization is added to the mix. One step in the process where errors frequently happen is when medical coders translate services rendered to the correct billing codes. This translation depends on subjective analysis by the coder, and that individual interpretation typically produces a wide variety of coding and opens the door to errors. In addition to mistranslations and other innocent errors, provider abuse is also a concern in some cases. Though most billing errors are just that –– errors –– some providers have historical patterns of fraud and abuse. It can be difficult for payors to identify potential abusive billing practices since it requires extensive knowledge around billing data, medical procedures and provider trends. 
35 percent of the hundreds of thousands of workers’ compensation bills that we audited contained some type of billing error.
Types of Errors
Let’s take a closer look at the types of errors and abuse we see on medical bills related to workers’ compensation claims.
Simple Errors
First, let’s consider simple errors. These errors could easily occur in the translation phase. Though simple, these types of errors are still difficult for payors to catch and could ultimately cost tens of thousands of dollars per bill, depending on the type of error.
- Data entry errors
- Unbundling of services
- Upcoding of procedure codes
- Inaccurate bill types
Complex Errors
Sometimes, the inaccuracies on bills can be even more complicated and difficult to identify. Split billing is one example of a complex error that can occur across multiple scenarios and services. This specific error frequently emerges when a provider separates surgery codes from medical supplies during billing. Although service charges include supplies, separate billing sometimes results in payment of both when the separate charge should be denied. This can be especially difficult for a provider to catch because it occurs across multiple different bills. A split bill, like most billing issues, may fall into one of two categories: an error or an abuse. Split billing is considered an error when coders do not understand the appropriate process to submit a bill correction to include additional services. Without proper knowledge of the standard rules for adjusting a bill, a biller may unintentionally re-bill or bill incorrectly. On the other hand, some providers deliberately separate charges with the intention of receiving a higher level of reimbursement than should be billable. This example would be considered an abusive billing practice.
How to Avoid Paying for Mistakes
To help avoid this scenario, payors can use a robust, automated auditing platform to help improve medical review efficiency and cost containment. An auditing technology platform can quickly sort through bills, make edits where appropriate and pass along a limited number of complex bills for a more detailed review by nurses. By adding an advanced technical auditing solution to the claims workflow, payors can feel confident in their process to catch errors and abuses in billing, which helps them stop paying for mistakes.
Up Next in the Series: In the next article, we will explain how an auditing solution works and the value it can add to a workers’ compensation payor’s workflow.



