Part Two: Evaluating In-Network and Out-of-Network Trends
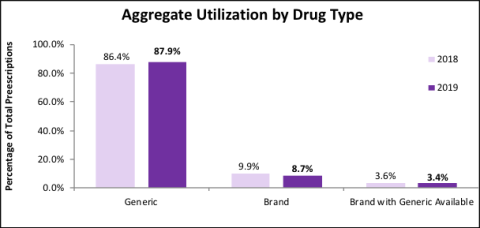
In this final post related to our in-network and out-of-network analysis we are taking a closer look at brand and generic medication trends in workers’ comp. Stay tuned for more posts addressing specific trends highlighted in the next piece of our drug trends series focusing on opioids. Generic medications are drugs made to work exactly the same way as brand name medications with the same active ingredients as the brand name product. The use of generic medications as a percentage of all medications dispensed continued its upwards trend over the past decade and accounted for 87.9% of all medications in 2019 versus 86.4% in 2018. Moreover, the use of brand medications fell by 1.2% and the use of brand medications with generic availability decreased by 0.2%.
Drug classes such as opioids or compounds continue to demonstrate decreased use year-over-year. It is also important to look at other drug types as prescribers look for alternative treatment options. Anticonvulsants (#3 in cost by drug type) are typically used for seizures but in many workers’ compensation cases they are used in managing pain, especially chronic or neuropathic pain. They had a 3.5% decrease in cost per script. This was largely driven by Lyrica®, due in part to its falling price and its’ associated generic which became available in mid-2019.

Another class to highlight from our drug trends analysis is the Hematological class. These medications include those treating blood disorders, especially for the prevention or treatment of blood clots such as Xarelto®, Eliquis®, or Lovenox®, which represent the top 3 medications in the class by both use and spend in 2019. This class jumped from #14 in cost in 2018 to #10 in 2019, coupled with a 12.8% increase in cost per script. The increase for these medications may be due in part to older workers, which are at greater risk for conditions leading to heart attack or stroke, along with the decreased use of warfarin. Notably, the newer anti-coagulation agents of Xarelto®, Eliquis®, and Pradaxa® are only available in brand name formats and do not contain many of the drug interactions and dietary restrictions seen for warfarin. Overall, the generic efficiency in 2019 increased from 96.0% to 96.3%. Working with your Pharmacy Benefit Manager (PBM) combined with a robust clinical program for injured worker populations can help determine appropriateness of medication therapies. As the need to control more than just the cost of workers’ comp prescription medications becomes increasingly apparent, one of the easiest ways to optimize cost savings while providing appropriate care is to ensure utilization of generic medications.


