NOTE: This survey was conducted prior to the COVID-19 pandemic. We wanted to know: What does the industry think is next in workers’ compensation and how will technology affect our industry in 2020 and beyond? How does the outlook for technology in our industry compare to the industry’s perspective in 2017, when Mitchell conducted a similar survey? To find out, we conducted a survey of about 100 workers’ compensation industry professionals.
Summary of Results
The results of the 2020 survey demonstrated that the adoption of technology is now, more than ever, at the forefront of the evolution of workers’ compensation claims management, and is a trend expected to continue and grow into the foreseeable future. Claims organizations and other businesses throughout the industry are relying on technology to help them solve a variety of challenges, but most importantly cost containment, efficiency and helping injured employees get back to health in a timely manner. Here is a summary of a few of the most interesting findings from the responses we received:
- About 50 percent of respondents said cost containment is the driving factor for adopting advanced technologies, such as artificial intelligence, predictive analytics, telemedicine, wearables, mobile and chatbots.
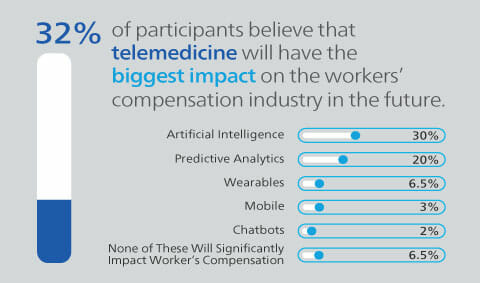
- Many respondents believe that telemedicine will have the biggest impact on the industry within the next five years (32%), followed closely by artificial intelligence (30%) and predictive analytics (20%).
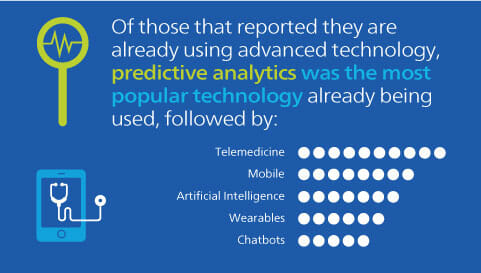
- Of those who said their organizations have already adopted these technologies, most respondents said they are using predictive analytics in their operations today, followed by telemedicine and mobile.
While this survey was conducted prior to the COVID-19 pandemic, we anticipate that these trends are still applicable today, with an additional growing emphasis on telemedicine, which is playing a large part in getting injured workers care during this time.
Breaking Down the Responses
1. Which technology do you think will have the biggest impact on the workers’ compensation industry in the next five to 10 years?
More than half of workers’ compensation professionals believe that telemedicine (32%) and artificial intelligence (30%) will have the greatest impact on the workers’ compensation industry in the next five to 10 years. This finding aligns well with participants reporting that the main drivers of technology adoption in the industry today are containing costs, increasing automation and helping workers’ get back to health, as both artificial intelligence and telemedicine can help organizations solve many of these goals.
In our 2017 survey, telemedicine came out on top, but with a much larger plurality (45%). Artificial intelligence came in second in the 2017 poll as well, but only received 19 percent of the vote. The rising importance of artificial intelligence from 2017 to 2020 indicates growing awareness that smart technology can automate many of the manual and rote processes that are typical in workers’ compensation claims workflows. Additionally, as the COVID-19 situation continues to evolve, we anticipate that respondents would continue to put a stronger emphasis on telemedicine as a workers' compensation technology that will have a big impact in the future, as this technology has increased in popularity to help injured workers get care during the pandemic and many states have loosened their regulations to allow for more telemedicine practice.
2. How likely is it that your organization will adopt advanced workers' compensation technology in the next five years?
It is clear from the survey that the workers’ compensation industry has already begun to adopt advanced technologies, with about 20 percent of respondents reporting that their organization has already implemented either telemedicine, artificial intelligence, predictive analytics, wearables, mobile or chatbots. This was a 50 percent increase from the 2017 survey, where only 10 percent of respondents said their organization was currently utilizing one of these technologies, demonstrating that the use of technology has expanded significantly in the industry just over the past three years. As a result of the coronavirus pandemic and surrounding regulations and guidelines, organizations may begin to incorporate even more technology now and into the future as they update and strengthen their business continuity plans. In the 2020 survey, a total of 94 percent of respondents said that their organizations are at least moderately likely to implement one of these technologies in the next five to 10 years, signaling that these technologies will continue to play a bigger role in the claims process. This finding was on par with the 2017 survey, in which 92 percent of respondents reported they would be at least moderately likely to implement one of these technologies.
3. If you selected “already using” as your answer to question two above, please specify which technologies your organization currently uses.
While the majority of participants reported that telemedicine and artificial intelligence will be the most likely to make the biggest impact on the industry in the coming years, predictive analytics is the technology that most organizations are using today. Next, respondents reported that their organizations have implemented telemedicine, followed by mobile. Today amidst the coronavirus situation, we anticipate that more claims organizations would report that they are using telemedicine in some format. Mitchell product and technology leaders Mike Bishop and Courtney Chandler provided some insight in an mPower article, sharing how predictive analytics can be used in the claims process: “Predictive analytics provides the ability and power to manage claims more accurately. We can use information from years of past claims to build models that will predict what may happen next in a particular claim. The models relate similar data points to the current claim and provide an adjuster insight into what may happen over the lifecycle of that claim.” As insurers continue to adopt predictive analytics and other technologies like telemedicine and mobile, they will continue down the path of making it easier to support injured workers and get them back to health quickly.
4. Which of these factors do you think is the most influential reason the workers' compensation industry is adopting advanced technologies?
Cost containment continues to be overwhelmingly the driving factor behind the workers’ compensation industry’s adoption of technology (2020: 47%, 2017: 54%). As the industry faces increasing pressures to contain costs, advanced technologies can help claims organizations to make both operational improvements and manage medical spend. For example, artificial intelligence can be used to surface key claim information, allowing adjusters to see the full picture and therefore make more informed decisions that could lead to improved accuracy and consistency.
Additionally, respondents reported that safety and risk management were additional drivers of workers' compensation technology adoption, aligning well to the industry trend of shifting the focus back onto the injured worker.
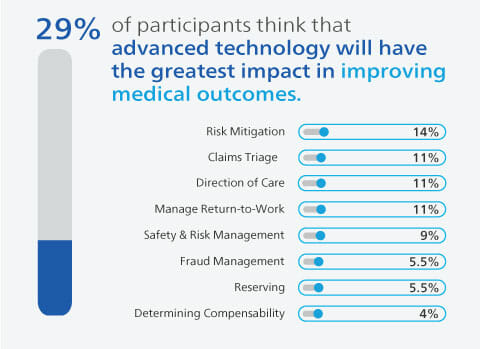
5. As it relates specifically to workers’ compensation claims operations, which of these areas do you think advanced technologies will influence the most?
Within the workers’ compensation claims process itself, advanced technology is expected to be the biggest help in improving medical outcomes (29%). This finding shows that organizations are looking to workers' compensation technology to help them find innovative ways to improve medical treatments, utilization and more. Some respondents also thought that technology will have a major influence on risk mitigation (14%) and claims triage (11%).
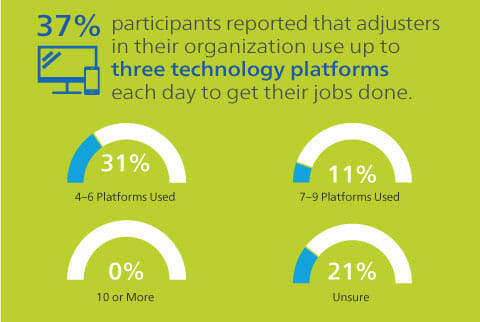
6. How many technology platforms do adjusters in your organization have to use every day to get their job done? (i.e. claims management, bill review, PBM etc.)
More than two-thirds of survey participants reported that adjusters in their organizations are using up to six technology platforms every day to complete their jobs. While it is great to see that adjusters are using workers' compensation technology and software to automate processes and support decision making, adopting multiple disparate platforms can also create additional challenges for adjusters. Over the next few years, we expect that claims organizations will shift to providing a single portal with all of the functionality that adjusters need in order to accomplish their tasks, helping to improve automation and make it easier to see the full picture and simplify the entirety of a claim.
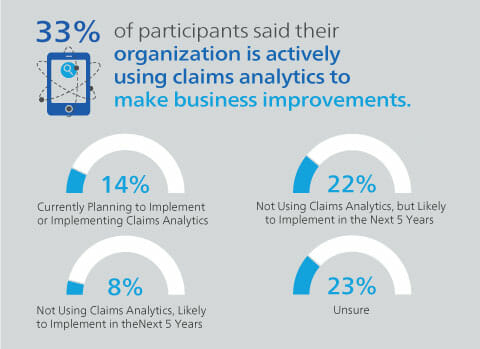
7. Is your organization currently using claims analytics to make business improvements?
About a third of survey respondents said they are already using claims analytics to make business improvements, with another 36 percent reporting that they are currently implementing or planning to implement analytics in the next five years. Many companies are currently using and will continue to adopt analytics in order to help them improve workflow efficiency, lower costs and help injured employees get back to work faster. As analytics capabilities improve and the decision-making process becomes more automated, adjusters can begin to re-focus their time from absorbing and interpreting mountains of data to problem-solving for injured workers.
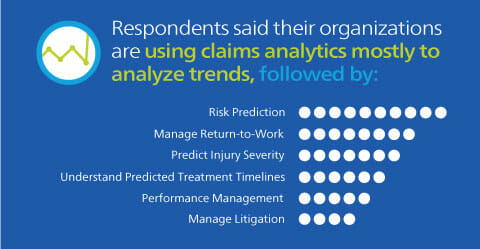
8. Which areas of claims processing are or will your company use claims analytics to support?
There are many applications for analytics in the claims process, especially with more data becoming available with the expansion of technology. Participants reported that they are currently using or planning to use claims analytics mostly to analyze trends, followed by predicting risks, managing return to work and predicting injury severity. We expect that as more data becomes available, more organizations will begin using analytics to not only observe trends but to provide insights that can improve the claims process in real-time.
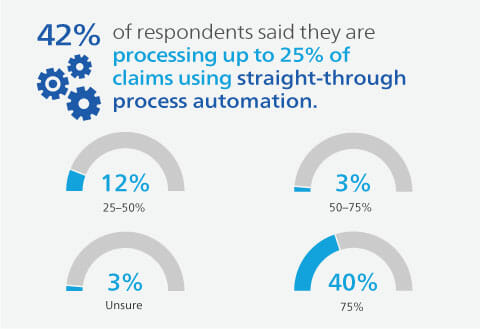
9. What percent of claims are processed in your company using straight-through process automation?
Many respondents (42%) reported that their organizations are processing about 25 percent of their claims with straight-through process automation. Only 18 percent of respondents said they were automating more than 25 percent of claims. This shows that today, there is a large opportunity for automation in workers’ compensation claims. While it is important that claims organizations strike the right balance between automation and the human touch to make sure they are doing the right thing for injured workers, organizations should look to reduce thresholds for straight-through processing in order to free up time for adjusters and allow them to focus on their core duties. Automation also can help improve both accuracy and consistency for small dollar bills or frequently submitted codes.
10. Which of the options below is the biggest claims challenge your organization is facing today?
The biggest challenge that workers’ compensation claims organizations are facing today is workflow consistency (27%), according to survey respondents. As the industry finds ways to overcome this challenge, technology and automation will continue to become more important in this process. As reported earlier, survey respondents believe that artificial intelligence will begin to play a bigger role in the claims process in the next five years, hopefully helping organizations to overcome the need for improved efficiency. Additionally, the industry is looking for ways to contain costs (19%) and manage employee turnover (15 percent).
Survey Demographics
Mitchell surveyed nearly 100 workers’ compensation professionals at a range of companies, including insurance carriers, third-party administrators, public entities, brokers, and managed care and risk management companies.